Physician career satisfaction has declined since the mid-1990s, and managed care gets much of the blameInstant Poll). Doctors associate managed care with:
- loss of autonomy3
- increased paperwork
- less time with patients
- frustrating phone calls with insurance company representatives.
Patients come to us with many types of medical insurance, and we often are unsure if they have adequate coverage. The stakes are high; career satisfaction and practice viability depend on prompt reimbursement without hassle, and successful outcomes depend on patients getting the care they need.
The “pitfalls” of managed care in mental health practice can be minimized, however. This article describes how to decrease the frustration, time, and effort you spend obtaining authorizations and receiving reimbursement.
Case manager: Nurse or social worker employed by a health maintenance organization (HMO) who processes, reviews, and authorizes claims. Can play a clinical role with severely ill patients, helping to coordinate their care, enrolling them in wellness or disease management programs, or advocating for them within the medical system.
Claims review: Method of reviewing an enrollee’s health care service claims before reimbursement. Purpose is to validate the medical necessity of provided services and ensure that cost of service is not excessive.
Medical necessity: Services that: 1) are appropriate and necessary for diagnosis or treatment of a medical condition; 2) are provided for diagnosis and treatment of a medical condition; 3) meet standards of good medical practice within the medical community; and 4) are the appropriate level of intensity to meet the patient’s need.
Summary plan description (SPD): Document developed by an employer or government entity that details an insurance plan’s medical insurance benefits and coverage limitations.
Third-party payer: HMO or other managed care entity that administers a health care plan and arranges for payment of medical services. Clinicians are the “first party,” and patients are the “second party.”
Utilization review (UR): Prospective, concurrent, or retrospective review of medical care for appropriateness of services delivered to a patient. In hospitals, includes review of admissions, services provided, length of stay, and discharge practices. UR usually involves protocols and guidelines to track, review, and render opinions about patient care. Claims for care that fall outside these guidelines risk being denied.
Managed care primer
Understanding how managed care works can help you develop more positive interactions with these systems. Managed care exists to help control medical costs. Restricting services is one method of medical cost control, but employers and government payers also are interested in improving disease prevention, recognition, and management.
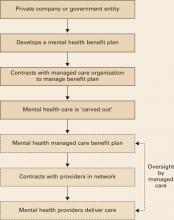
Delivering health benefits. The process begins when a business or government entity develops a summary plan description (SPD) (Box 1), defining what medical and mental health care services a policy covers (Figure).
A managed care company—typically a health maintenance organization (HMO) or similar entity—enters into a contract to implement and manage health care benefits for all persons covered by the plan. Because of their complexity, mental health services are usually “carved out” (Box 2)4 to a mental health specialty managed care company.
Utilization review. Whenever you deliver mental health care, your claims and treatment plans are scrutinized through utilization review (UR). Before authorizing payment, reviewers typically screen claims to:
- verify that the patient’s benefit plan covers the service
- establish the service’s medical necessity
- ensure that the treatment meets accepted standards of care.
UR staff in most managed care companies have administrative authority to authorize care, but care can be denied only by a medical director—typically a psychiatrist who reviews the clinical information submitted by the provider.
Figure Model of a typical managed care plan
Example 1
Claim authorization. A psychiatrist evaluates a patient and diagnoses major depression. The psychiatrist submits a treatment plan to the managed care company requesting authorization for 6 medication management and 10 psychotherapy sessions for the next 12 months. A UR representative reviews the plan, verifies the patient has appropriate coverage, and authorizes the sessions.
Example 2
Claim denial. A psychiatrist evaluates a patient and diagnoses major depression. The psychiatrist submits a treatment plan to the managed care company, requesting authorization for 10 EEG biofeedback sessions to treat the depression. A UR representative examines the plan and asks the medical director to review it. The medical director denies authorization because EEG biofeedback does not meet accepted standards for depression treatment.
Negotiating exceptions. Managed care companies must follow the letter of the benefits they administer. Some employers, however, allow for a “benefit exception” when practitioners identify patient services not covered under the benefit that, if implemented, might improve care and reduce costs.
If you encounter a situation where you believe plan limitations might adversely affect patient outcome and expense, point it out to the managed care company and ask if the patient’s plan allows benefit exceptions. Some plans do not allow for partial hospitalization, for example. If a patient with frequent inpatient admissions could be cared for in the less-intensive environment of a partial hospital program, the managed care case manager might approach the employer and suggest a benefit exception for this patient.