When a patient with major psychiatric illness exhibits violent behavior, consider the course of violence in relation to his or her fixed and changing symptoms and deficits.1,2 Although most patients with schizophrenia, major depression, or bipolar disorder are not violent, effectively treating those who are calls for:
- differentiating between transient and persistent violent behavior
- providing medications and nonpharmacologic interventions shown to reduce each behavior
- addressing substance abuse and violent behavior concurrently.
Is violence transient or persistent?
Violent behavior is a common reason for psychiatric admission and prolonged hospital stays3 and a barrier to appropriate community placement4 and successful community reintegration.
Transient violence is limited to an acute psychotic episode; as psychotic symptoms abate, the violence resolves. Delusions, hallucinations, and conceptual disorganization are key triggers of transient violence.5 Excitement, anger, and agitation are its prominent symptoms.6
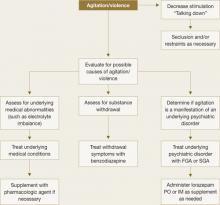
Treat a patient experiencing an acute violent episode with an oral first- or second-generation antipsychotic. For acute agitation, intramuscular (IM) delivery provides more rapid symptom resolution (Table 1). IM ziprasidone is approved for agitation associated with schizophrenia and IM olanzapine for use in agitation associated with schizophrenia or bipolar mania. Try talking calmly to the patient and explaining the need for medication (Figure 1). If this is not possible, a show of force might induce the patient’s cooperation.7
For sedation, antipsychotic medication can be supplemented by lorazepam, the only benzodiazepine that is reliably absorbed when administered IM. Lorazepam has a relatively short half-life, and the usual dosage of 1 to 2 mg can be administered orally, sublingually, intramuscularly, or intravenously every 1 to 6 hours. Exercise caution, however, when respiratory depression is a possibility.
Table 1
Medications used to treat violence on an emergency basis
| Drug | Route of administration* | Recommended dosage† |
|---|---|---|
| Benzodiazepines | ||
| Lorazepam | IM or PO | 1 to 2 mg IM or PO |
| Midazolam | IM | 5 mg |
| First-generation antipsychotic‡ | ||
| Haloperidol | IM or PO | 2 to 7.5 mg IM or PO |
| Second-generation antipsychotics‡ | ||
| Olanzapine | IM or PO | 10 mg IM or PO |
| Risperidone | PO | 2 to 6 mg |
| Ziprasidone | IM | 10 to 20 mg |
| * Use oral medication if patient is cooperative; otherwise use an intramuscular injection. | ||
| † Lower dosages are used for elderly patients or those with dementia. | ||
| ‡ Antipsychotics are not recommended for aggressive patients without a psychotic disorder or bipolar mania diagnosis. | ||
Figure 1 Managing patients who present with acute violence or agitation
FGA: First-generation antipsychotic; SGA: Second-generation antipsychoticPersistent violence. Emotional turmoil is usually less pronounced in patients whose violence is persistent.8 Neurocognitive impairments, antisocial traits, and specific psychotic symptoms may exist singly or in combination in patients prone to persistent violence.
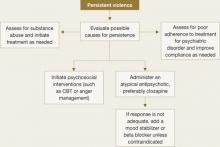
When a patient continues to be violent, consider poor treatment adherence or substance abuse, especially with outpatients (Figure 2).
Figure 2 Managing patients who exhibit persistent violent behavior
Neurological and neurocognitive impairments are associated with persistent violence. Fairly broad impairments in various domains are seen on a variety of tests. Patients with neurocognitive impairment often present with impulsivity9 and deficits in behavioral adaptability.
In general, the consequences of a behavior determine its course; assaultive behavior usually decreases rapidly when strongly discouraged. Violent behavior that persists, therefore, suggests that neurocognitive impairment is causing a failure in behavioral adaptability.
Psychopathy, antisocial traits, and antisocial personality disorder (APD) also can result in persistent violence.
Antisocial personality is defined primarily by behavioral symptoms such as irresponsibility and criminal activities. Psychopathy also includes these symptoms but adds interpersonal and affective impairments such as callousness, grandiosity, and lack of remorse.
Psychopathy was the strongest clinical predictor of violence in a large trial of outpatients with major psychiatric disorders.10 APD, on the other hand, was the most significant clinical predictor of violent recidivism among offenders with mental illness in a meta-analysis of predictive longitudinal studies from 1959 to 1995.11 In another study, psychopaths were about 5 times more likely than nonpsychopaths to engage in violent recidivism.12
In addition to recidivism, the violence associated with psychopathy is characterized by its severity. Violence in these patients is often premeditated, deliberate, and goal-driven.
Persistent psychotic symptoms also play an important role in persistent violence and may represent treatment resistance. Some specific delusions, for example, are more likely to lead to violence and may persist despite overall improvement in psychotic symptoms.
Link et al13 have proposed that violence is more likely when a person has “threat/control override” delusions—if he believes people are seeking to harm him or outside forces are controlling his mind.
Junginger stressed that violent themes in a patient’s delusions are important predictors of violence.14 Delusions associated with violence are often chronic and well-circumscribed.