Discuss this article at www.facebook.com/CurrentPsychiatry
Mrs. B, age 45, is referred by her primary care physician (PCP) for treatment of depressive symptoms that have worsened over the last 6 months. Her depressed mood is associated with worsening of multiple chronic, physical symptoms that began 4 years ago with several musculoskeletal complaints. Three years ago she developed recurrent abdominal discomfort and bloating, followed by recurrent chest pain. These symptoms have resulted in multiple trips to the hospital, several invasive procedures, and extensive medical consultation. After repeated workups, her symptoms are medically unexplained. These symptoms interfere with her ability to engage in and enjoy life.
Even after thorough investigation, up to one-third of patients’ physical symptoms remain unexplained.1-3 Most patients with unexplained symptoms improve; however, a small proportion do not. Such patients often are referred for psychiatric consultation.
Workup may reveal psychiatric etiology of a patient’s medically unexplained physical symptoms (MUPS). Clinicians need to take a unique approach to caring for patients whose symptoms remain unexplained after workup because diagnostic features may emerge over time and a collaborative, unbiased, integrated approach eventually may reveal a treatable diagnosis. This type of approach also is important when no medical or psychiatric diagnosis can be reached.
This article reviews the prevalence, comorbidity, and treatment challenges of patients whose physical symptoms are medically unexplained, and recommends evidence-based treatment strategies.
Inconsistent terminology
The terms MUPS, medically unexplained symptoms, somatoform disorder, somatization, and the functional syndromes (eg, irritable bowel syndrome [IBS], fibromyalgia, interstitial cystitis, chronic fatigue, etc.) often are used interchangeably. This inconsistent nomenclature creates classification difficulties because several of these terms assume a different etiology for the patient’s physical symptoms (ie, medical vs psychiatric).
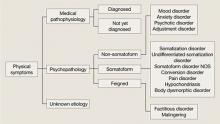
Physical symptoms typically are explained by:
- medical pathophysiology
- psychopathology, or
- unknown etiology (Figure).
MUPS typically are defined as physical or somatic symptoms without a known etiology after appropriate testing, workup, and referrals. Workup may be limited or extensive, may evolve over time (eg, diagnosis may be made 2 years after primary symptom onset), and often involves collaboration among several specialists.
The above definition does not specify severity, medical/psychiatric comorbidity, or number or duration of symptoms. A proposed classification, medically unexplained symptoms spectrum disorder, attempts to categorize patients with MUPS based on severity and duration of symptoms, as well as medical and/or psychiatric comorbidities (Table).4 MUPS may account for up to two-thirds of physical symptoms in specialty clinics; to read about the prevalence of MUPS, see the Box below.
Figure: Typical etiology of physical symptoms
NOS: Not otherwise specifiedTable
Medically unexplained symptoms spectrum disorder
| Severity | Mild, moderate, severe |
| Duration | Acute (days to weeks), subacute (<6 months), chronic (>6 months) |
| Comorbidity | Psychiatric, medical, none |
| Source: Reference 4 | |
CASE CONTINUED: Abuse and assault
Mrs. B has been married for 10 years and has 2 children. She denies using tobacco, alcohol, or illicit drugs. Both of her parents were in good physical health. As a child Mrs. B was physically and verbally abused by her father, and her parents divorced when she was 15. She was sexually assaulted while in college.
Mrs. B has had 1 previous depressive episode, which occurred shortly after the sexual assault. During that time she was hospitalized twice for attempting suicide by overdosing on prescription medications. She was stabilized on fluoxetine, 40 mg/d, which was tapered and discontinued after 2 years.
Factors linked to MUPS
Young women (age 16 to 25) are more likely to receive an MUPS diagnosis than men or older individuals. Employment, socioeconomic background, and educational level are not consistently associated with MUPS.5 Patients with MUPS have higher rates of physical and sexual abuse.6
Several studies have shown an association with childhood parental ill health and development of MUPS, but the exact nature of “ill health” was not clearly defined. Parental death was not associated with MUPS, which suggests that the association to parental ill health is related to non-threatening physical disease.6
Approximately 60% of patients with MUPS have a comorbid non-somatoform DSM-IV-TR diagnosis.7-9 Symptoms and rates of depressive, anxiety, and panic disorders are higher in patients with MUPS than either healthy controls or patients with similar diseases of known organic pathology.7,8