Alcohol dependence is not an acute illness. Progression from alcohol use to dependence typically takes years, and alcohol dependence is a chronic illness with symptom severity that increases over time.1,2 As the level of alcohol intake increases, the probability of developing an alcohol use disorder, cirrhosis, seizures, cancer, hypertension, stroke, and injuries significantly increases.3,4 Most alcohol-related harm occurs in high-risk drinkers who do not meet DSM-IV-TR criteria for an alcohol use disorder.5,6
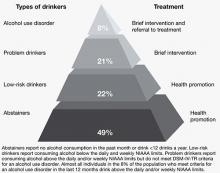
Clinicians therefore have an opportunity to intervene at early stages of alcohol use to help prevent progression to dependence and reduce harm. The concept of a continuum from low-to high-risk alcohol use is replacing the disease-oriented model that focuses on identifying and treating individuals who meet DSM-IV-TR criteria for alcohol use disorders (Figure 1).4,7 Efforts to provide screening and intervention earlier in the disease course have:
- mainly been carried out in the primary care setting
- been aimed at nontreatment-seeking, nondependent individuals
- led to recommendations for safe alcohol consumption limits.8-10
One of the largest outreach efforts is a federally funded screening, brief intervention, referral to treatment (SBIRT) program established in 17 states that targets hospital emergency rooms, community health centers, and trauma centers.11
Although research on the use of brief interventions for problem drinking in psychiatric settings is limited,12-15 psychiatrists can employ these strategies, even during a brief medication management visit.
Figure 1: Recommended treatment based on type of alcohol use
NIAAA: National Institute on Alcohol Abuse and Alcoholism
Source: References 7,16
How much is too much?
The National Institute on Alcohol Abuse and Alcoholism (NIAAA) recommends men age <65 drink no more than 4 drinks/day and no more than 14 drinks/week and women of any age and men age ≥65 drink no more than 3 drinks/day and no more than 7 drinks/week.16 A standard drink is defined as 14 grams of absolute ethanol (12 ounces of beer, 5 ounces of wine, or 1.5 ounces of distilled spirits). Drinking above these levels is likely to result in harm and is defined as hazardous or at-risk use.10,17,18 Harmful use is alcohol consumption that has resulted in adverse mental or physical effects.10,17,18 We use “problem drinking” to describe both at-risk and harmful use as alcohol intake that exceeds NIAAA-recommended limits but does not meet DSM-IV-TR criteria for an alcohol use disorder.
In the United States, approximately 20% of the population exceeds NIAAA recommended alcohol intake guidelines without meeting criteria for an alcohol use disorder.18 Problem drinkers have an increased risk of developing an alcohol use disorder, nicotine dependence, liver disease, financial problems, marital disruptions, injuries, and driver’s license suspensions.4-6,19
Problem drinking is common in psychiatric populations and may lead to difficulties beyond those experienced in the general population.20,21 For example, problem drinking in individuals with bipolar disorder is associated with reduced medication compliance, greater functional impairment, and possibly more suicide attempts.22,23 Even moderate alcohol use below the NIAAA-recommend levels may increase symptom severity in patients with bipolar disorder.22,23
Interviewing techniques
Interventions to identify and treat problem drinkers have focused on the primary care setting because these physicians often are the only medical professionals problem drinkers encounter.8-10 The style of counseling is based on motivational interviewing. Providers use therapeutic empathy, describe risk, deal with ambivalence and resistance, assess motivation to change, emphasize patient responsibility and self-efficacy, and provide a menu of specific strategies to reduce alcohol use. However, unlike standard motivational interviewing, in brief interventions, providers use clear, directive advice to reduce alcohol consumption in the context of the medical provider role. Brief interventions also draw on cognitive-behavioral therapy and general education strategies utilizing contracting, goal setting, and written materials such as self-help manuals.24
Clinicians’ time demands have driven an effort to make interventions for problem drinkers efficient and time-limited. A single short intervention (5 to 15 minutes) can be effective, but 2 to 4 sessions of 5 to 15 minutes each seems to be more effective.8,10 The emphasis is on increasing a patient’s insight and awareness of risk to prompt him or her to establish and manage a goal to reduce alcohol intake. As opposed to abstinence, which is commonly recommended for patients with alcohol use disorders, reducing intake typically is encouraged for problem drinkers.9,10,16,18 For patients who use alcohol over the recommended limits and also meet criteria for an alcohol use disorder, clinicians can deliver a brief intervention, but should recommend abstinence from drinking and provide referral for further treatment.9,10,16,18