Pegylated interferon-alpha with ribavirin is the most effective therapy for chronic hepatitis C infection,1,2 but psychiatric patients often discontinue IFN-alpha because of its mood side effects.3 Most studies describe depressive states, although manic symptoms—irritability, aggression, anger, hostility, emotional lability, anxiety, panic attacks, and insomnia—also have been reported.4-6
To help you manage adverse mood changes and prevent IFN-alpha treatment discontinuation in patients with hepatitis C, this article:
- reviews studies of patients with a history mood disorders who were treated with IFN-alpha
- explains how to recognize and treat IFN-alpha-induced mood disturbances when antidepressants are contraindicated.
Psychiatric Patients and IFN Therapy
Chronic hepatitis C infection is common among psychiatric patients. Routine screening among 1,556 patients admitted to a U.S. public psychiatric hospital across 3 years identified 133 patients (8.5%) who were positive for hepatitis C virus.7
Patients with psychopathologic symptoms before starting IFN therapy may suffer more-severe adverse psychiatric effects during treatment than those without psychopathology.8 In fact, mood disorders were considered an absolute contraindication to IFN therapy until recently.
Now that the National Institutes of Health (NIH) has recommended extending hepatitis C research and treatment to psychiatric patients, IFN-alpha-induced mental illness could become more common in clinical practice. Before the 2002 NIH consensus statement, patients with mental illness and substance use disorders—who represent >50% of candidates who need IFN therapy—were excluded from research protocols.
Safely using IFN. Some reports and studies suggest that patients with past or existing psychiatric disorders can be treated safely and effectively with IFN-alpha.
In a prospective open-label study, 29 of 31 patients with co-existing chronic hepatitis C and psychiatric illness completed 6 months of IFN therapy, 5 million units (MU) three times/week or 5 MU daily. Patients continued maintenance psychotropics during IFN treatment, and a psychiatrist monitored psychiatric symptoms.
Psychiatric illness worsened in four patients, and two discontinued IFN treatment. Serum alanine aminotransferase returned to normal in 22 patients (71%), and hepatitis C virus RNA cleared from the sera of 15 (48%).9
Another prospective study of 50 patients treated with IFN for chronic hepatitis found that those with a pre-existing mood or anxiety disorder were not more likely than others to discontinue IFN therapy.10
Unique to hepatitis therapy? IFN-induced mood disturbances are probably different in patients with chronic hepatitis C than in those receiving IFN for other diseases because of differences in regimens and effects of the underlying pathologies. For example, prescribing a preventative antidepressant before starting IFN treatment might help cancer patients but not patients with hepatitis C.11
This distinction could be particularly important when giving IFN-alpha to patients who are vulnerable to psychiatric illness with impulsive features. To emphasize this point, we describe clinical features and treatment response in patients with hepatitis C who were treated in our department.
IFN-Alpha-Induced Moods
In our prospective study of 93 patients, 30 (32%) developed IFN-alpha-induced mood disorders during the first 12 weeks of treatment.12 Contrary to previous studies focusing on depression, most of our patients had a mix of manic/hypomanic and depressive symptoms. Twenty-four (13 women and 11 men, mean age 43) accepted referral to a psychiatrist specializing in mood disorders to characterize their symptoms.
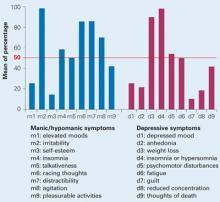
Mood characteristics. Using DSM-IV criteria, the psychiatrist determined that IFN-alpha induced both manic/hypomanic and depressive symptoms in many patients, and the manic/hypomanic features predominated. Five manic symptoms and three depressive symptoms were present in >50% of patients (Figure 1, Table 1).
Three patients presented with a manic episode,15 with hypomania with prevalent irritability and dysphoric features, and 6 with a mixed depressive state (major depressive episode with at least 3 hypomania symptoms).13 Four patients (17%) suffered a relapse of alcohol or cannabis abuse.
Nearly all (84%) reported paroxysmal anxiety, and all had emotional hyperreactivity that the psychiatrist described as a main symptom of a manic or mixed state.14 Most felt extremely impulsive and feared losing control. Two faced legal difficulties, and one was in prison.
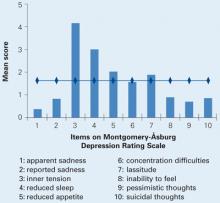
The patients’ mean Montgomery-Åsburg Depression Rating Scale (MADRS) score was 16.12 (±1.6), indicating a mild to moderate depressive state. The highest-scoring items were inner tension, reduced sleep, reduced appetite, and lassitude (Figure 2).
Their mean Bech-Rafaelsen Mania Scale15 score was 14.33 (±1.3), indicating hypomanic or moderate manic symptoms. Hostility was by far the predominant manic symptom (mean score 3.2/4). Other manic symptom scores ranged from 0.2/4 to 2.1/4 (Figure 3).
Figure 1 Mood symptoms identified in 24 patients after 12 weeks of IFN-alpha treatment
IFN: Interferon
Source: Reference 12
Figure 2 Depressive symptoms in 24 patients with IFN-induced mood disorder
IFN: Interferon
Source: Reference 12