‘Immediately after the event I was a wreck. I vaguely remember talking to the family; I don’t know if I was much use to them. … That night I got drunk. It was the only way I could sleep. A sensitive colleague came and sat with me.”1
Besides being targets of malpractice suits, psychiatrists also serve as resources for colleagues who are sued. Specific actions can help you and those you counsel deal with the stress of an adverse event before and during litigation. Remember that:
- anticipation is the best defense
- knowledge is power
- action counters passivity
- a supportive environment is essential.
ANTICIPATING LITIGATION
What is the risk? No nationwide reporting system tracks the incidence of medical malpractice claims, but industry experts suggest a claim is leveled against 7% of psychiatrists each year.2 The risk is higher for other medical specialists: a recent survey by the American College of Obstetricians and Gynecologists found that 89% of practicing ObGyns had been sued at least once in their careers.3 Because a claim usually takes several years to resolve, a substantial number of physicians—including psychiatrists—are involved in litigation at any one time.
Successfully anticipating litigation begins with being familiar with your state’s statute of limitations—usually 2 to 3 years after discovery of the incident, with exceptions for children, the disabled, and designated special circumstances. If a plaintiff’s case is not filed within this time, a disputed outcome can never be the subject of a malpractice claim.
Adverse events. The severity of the outcome, the nature of your relationship with the patient, and the degree of your responsibility for an adverse event contribute to the intensity of your initial emotional response. If a mistake caused the event, your reaction may be even more severe.4-6 Whatever the event’s specifics, you may ruminate about your role and degree of responsibility (Table 1).
Table 1
Nagging questions after a ‘bad’ patient outcome
|
Expect that your view of the circumstances will generate a complex array of feelings: shock, anxiety, depression, shame, guilt, self-blame, disbelief, self-doubt and inadequacy, anger, and even relief from not having to work with a difficult patient anymore.
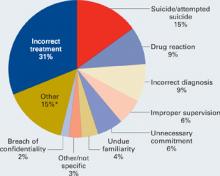
Patient suicide. More than one-half of psychiatrists and up to one-third of psychiatric residents experience a patient suicide.7-10 The Joint Commission on Accreditation of Healthcare Organizations reports that suicide is the most frequent sentinel event, representing 501 (13.1%) of the total 3,811 sentinel events reviewed since 1995.11 Professional Risk Management Services, a major medical malpractice insurer of psychiatrists, reports that suicide and attempted suicide are the most frequently identifiable causes of liability payments (Figure).
Figure 1 Psychiatric claims by cause of loss in the United States, 1998 to 2005
Almost all lawsuits assert multiple allegations of negligence, and “cause of loss” represents the main allegation made in the claim or lawsuit. Thus, the category of “incorrect treatment” may be alleged in a lawsuit based on a patient suicide, but the main or chief allegation/complaint is stated as “incorrect treatment.” The most frequent identifiable cause of loss is suicide and attempted suicide.
* “Other” includes administrative issues, abandonment, premises liability, Tarasoff, third parties (such as parents), retained object, libel/slander, boundary violation, deleted duplicate file, Fen-phen, lack of informed consent, forensic issues, and miscellaneous.
Source: Prepared by Professional Risk Management Services, Inc. Reprinted with permission.
Psychiatrists’ feelings of distress after a patient suicide mirror the personal sense of failure and inadequacy most physicians feel when they are unable to prevent a patient’s death or serious injury. At the same time, we must:
- deal with the event’s medical complications, with relevant notifications and disclosures (Table 2)
- address the emotional pain of the injured patient or family
- participate in mandated reviews
- recognize and manage our emotional disruption (Table 3).
Table 2
Recommended medical steps, notifications,
and disclosures after an adverse event
| MEDICAL STEPS Take necessary actions to limit further injury or disability Obtain appropriate consultations Review the medical record; anticipate the patient’s follow-up needs and make recommendations for further treatment |
| NOTIFICATIONS Follow the health care system’s and insurer’s guidelines for notifying the patient/family Inform the institution’s risk manager and your professional liability carrier as soon as possible Write a description of the event for the record and a narrative for your personal file (and your lawyer’s) in case a suit is filed later Do not talk with the media |
| DISCLOSURES Acknowledge your ethical obligation to be truthful Follow your institution’s and insurer’s disclosure guidelines Expect to feel intimidated and uneasy in discussing your role in the event Expect the patient/family to be angry and disappointed in you Convey an interest in the patient’s/family’s emotional state; express sorrow for their loss Tell the patient/family what you know for sure; don’t speculate about what is not known, and don’t make false promises or false reassurances Don’t hurry; give the patient/family time to ask questions Expect to feel better after a truthful exchange |